Weight regain after gastric band removal and endoscopic Sleeve
Presentation:
In this video we describe the case of a 54 year old female patient who presented with weight regain after previous gastric banding, band removal and endoscopic sleeve gastrectomy in association with Barrett's esophagus. We decided to perform a conversion to a Roux-en-Y gastric bypass.
Clinical History:
- 1998: Lap. gastric banding. BMI 35 kg/m². Weight loss: from 84 kg to 45 kg, stable weight at 55 kg
- 2014: Lap. adhesiolysis, intraperitoneal repair of ventral hernia
- 2017: Band removal for dyspepsia, gastro-esophageal reflux
- 2018: Endoscopic sleeve gastrectomy for weight regain. Weight: 78 kg. No weight loss achieved after the procedure
- Current problem: further weight gain: Current state: 83,2 kg – 154 cm kg/m²: BMI: 35.1 kg/m²
- Lab tests: elevated cholesterol and triglycerides
- Pre-operative upper GI endoscopy: Barrett's esophagus C2M5, no esophagitis. Limited volume reduction of the middle part of the stomach. Proximal and distal stomach unchanged
- Biopsies: no dysplasia. No H. pylori
- Upper GI series: stasis of contrast in the distal esophagus, decreased diameter of the cardia, normal caliber of the antrum and body of the stomach. Small sliding hernia
Technique description:
Laparoscopic conversion of endoscopic Sleeve ( post-Lap. Band placement ) to Roux-en-Y gastric bypass.
Procedure Steps:
- 1. Trocars ( 5 ) placement
- 2. Adhesiolysis, opening of the fibrous capsule of the previous band. Cutting of the gastro-gastric sutures up to the angle of His by sharp dissection, by this unfolding the anterior gastric wall
- 3. Insufflation of the stomach by the anesthesiologist demonstrated the unfolded stomach
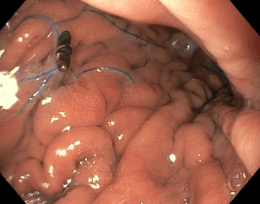
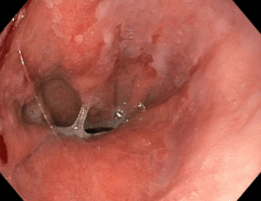
- 4. Identification of the endoluminal gastric sutures endoscopically as well as via laparoscopy. Some endoscopic stitches have been broken. We identify the most cranial suture and stay above and lateral to this point to create the pouch
- 5. Defining the entrance to the omental bursa at the lesser curvature
- 6. During dissection of the stomach, we found a small hiatal hernia with a wide open hiatus
- 7. Creation of the gastric pouch with a linear stapler leaving all the endoluminal stitches on the side of the remnant stomach
- 8. Creation of an opening in the distal / lateral part of the pouch
- 9. Purse string (PDS 3-0)
- 10. Insertion of anvil of circular stapler into the gastric pouch and tying of the purse string
- 11. Splitting of the greater omentum
- 12. Identification of Treitz’s ligament and measurement of biliary limb length (50cm)
- 13. Enterotomy and introduction of the circular stapler
- 14. Connection of the anvil and construction of the circular anastomosis (3.5 mm circular stapler height)
- 15. Division of the jejunum close to the GJ anastomosis
- 16. Creation of a stapled jejuno-jejunostomy (alimentary limb length 130 cm) using a linear stapler
- 17. Division of the blind loop
- 18. Hiatal hernia repared by cruroplasty with 2 non- absorbable stitches. Fixation of the fundus of the remnant stomach to the posterior side of the pouch and to the left crus with 1 non- absorbable stitch
- 19. Closure of the entero-enteral mesenteric gap en the Petersen’s space
- 20. Leak test negative
- 21. Hemostasis
- 22. Closure of the left lateral trocar port site's fascia (which was enlarged to introduce the circular stapler)
- 23. Positioning of an easyflow drain
- 24. Trocar removal, suturing of the skin
Learning Points:
- Unfolding the gastro-gastric sutures of the previous band and thereby restoring the anatomy of the gastro-esophageal junction is necessary in order to avoid stapling the stomach twice, thus reducing the risk of leak
- Intraoperative endoscopy is mandatory before creation of the pouch in order to exclude endoluminal stitches
- The advantage of the circular anastomosis is that it is made in a transverse plane, which allows the surgeon to incorporate only “healthy”, non-scarred and homogenous tissue