To access AIS Channel content, please allow all cookies. Please click here to configure your preferences.
Self-expanding metal stents (SEMS) , first developed in the 1990s, have evolved dramatically in recent decades. They were used mainly for the palliation of inoperable gastrointestinal malignancies but, in the last decade, their use as a bridge to surgery in cases of colorectal obstruction has been under debate.
Enteral stents can be divided into two types: uncovered and covered. Although covered stents reduce the risk of tumour ingrowth and can be used to treat fistulas, fully covered stents have less anchoring power and thus an increased risk of migration compared to uncovered stents.
SEMS can provide a good alternative to other therapeutic options for colorectal obstruction such as palliative surgery or radiation therapy. Several studies have shown the effectiveness of SEMS placement in patients with unresectable malignant colorectal obstruction and a reduction in the morbidity and mortality compared to surgical palliation. However, the risk of perforation in patients who received chemotherapy is well known, especially in those treated with bevacizumab, and thus palliative SEMS placement in these patients is still a matter of debate. If SEMS placement is to be considered in patients with a long life expectancy, a plan to address the potential long-term complications of SEMS placement should be formulated.
Up to 10-30% of patients with colon cancer will initially present with acute colonic obstruction. Traditionally, emergency surgery proceeded with no staging work up. This decompressive surgery carries significant risks of morbidity (32-64%) and mortality (15-34%) . In these cases, SEMS can be a good option for the treatment of acute malignant colonic obstruction as a bridge to surgery , allowing for preoperative evaluation and improvement of the patient’s medical condition. Some authors have reported a higher rate of primary anastomosis after SEMS as a bridge therapy than after decompressive surgery, with lower colostomy rates , shorter hospital stays, and fewer medical complications . Other groups have reported a higher local recurrence rate after SEMS compared to emergency resection, raising concerns about the risk of both local progression and metastatic spread.
A recent metaanalysis by Arezzo et al. confirms the lower short-term overall morbidity and lower rate of temporary and permanent stoma with stent-bridge-to-surgery compared to emergency surgery.
Approximately 32-54% of obstructing tumours are located in the proximal colon but only 5% of the reported cases of colonic stenting involve the proximal colon. A recent study by Amelung et al. found no differences in terms of morbidity and mortality between SEMS placement and emergency resection, but it did find a decrease in the temporary stoma rate in the SEMS group. It is reported to be a more demanding procedure because of the longer distance from the anus and the inability to prepare the colon since enemas only clean the distal bowel.
Several SEMS-related complications have been reported in the literature: re-obstruction, stent migration, stent-related perforation, bleeding. A s tent-related perforation rate of 2.4% in patients including both SBTS and palliative SEMS has been reported by Arezzo et al. with an increased rate of perforation (5.3%) in the SEMS palliative group (FIG.1, FIG.2 and FIG.3) . Some studies have reported an even higher perforation rate in patients treated with eGF-blocking agents such as bevacizumab and in these cases, SEMS is usually contraindicated. Migration rates of 7.3% and re-obstruction of 12.2% , increasing to 15.8% and 26.3% respectively in the palliative SEMS group have been reported.
In palliative patients , in which oncological outcomes are less relevant, the European Guidelines recommend s tent placement for left sided colonic obstruction as the preferred palliative treatment approach except when eGF-blocking agents (such as bevacizumab) are used due to the increased risk of perforation.
The use of SEMS as a Bridge-to-Surgery is associated with lower short-term overall morbidity , a lower rate of temporary and permanent stoma and a possible positive effect on quality of life compared to emergency surgery for left sided malignant colonic obstruction. However, data regarding tumour recurrence raises concerns about the oncologic safety of stenting .
In the case of malignant obstructions of the proximal colon , SEMS appears as a feasible and safe alternative for emergency resection if performed by an experienced endoscopist.
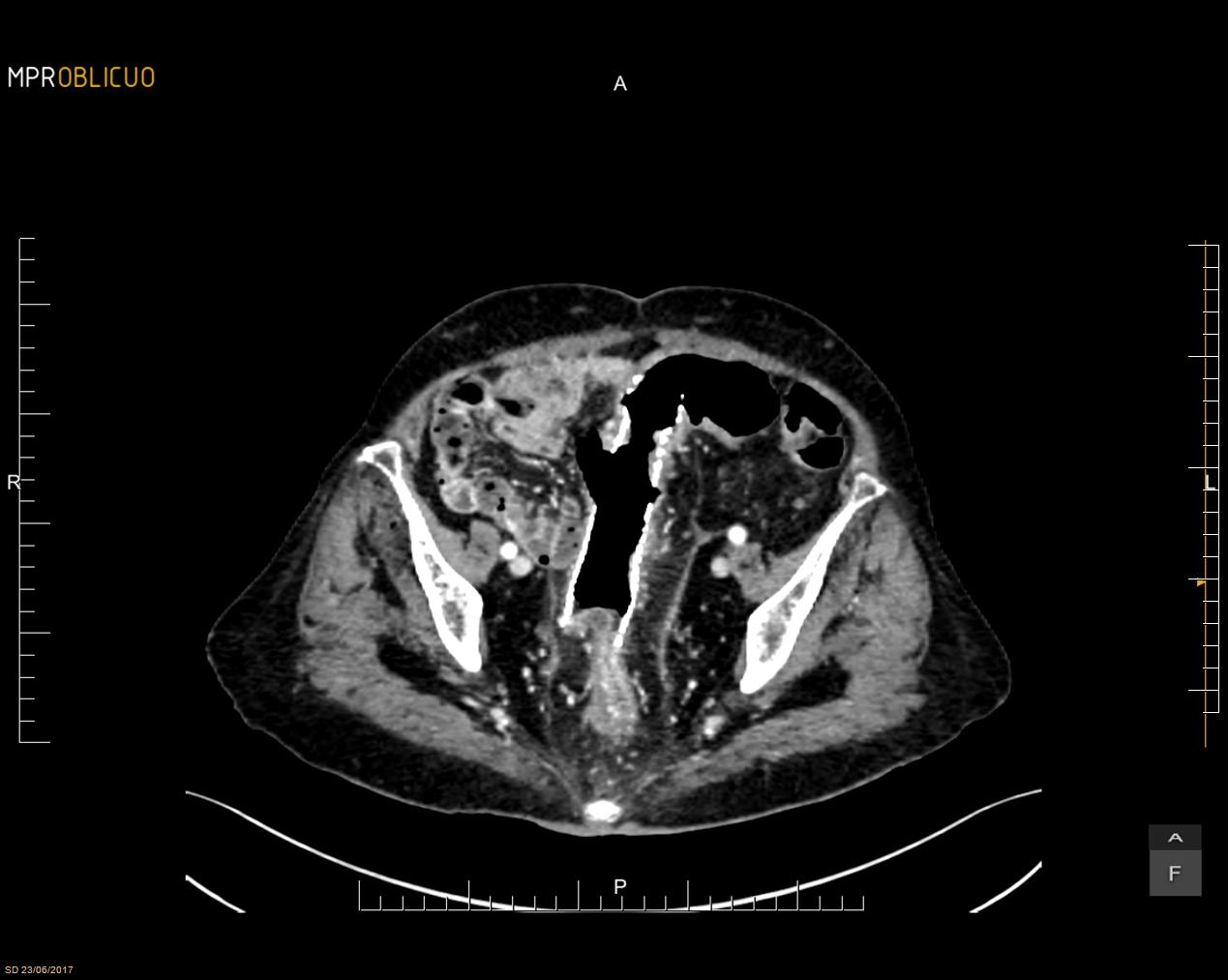 FIG 1.
FIG 1. FIG 2.
FIG 2.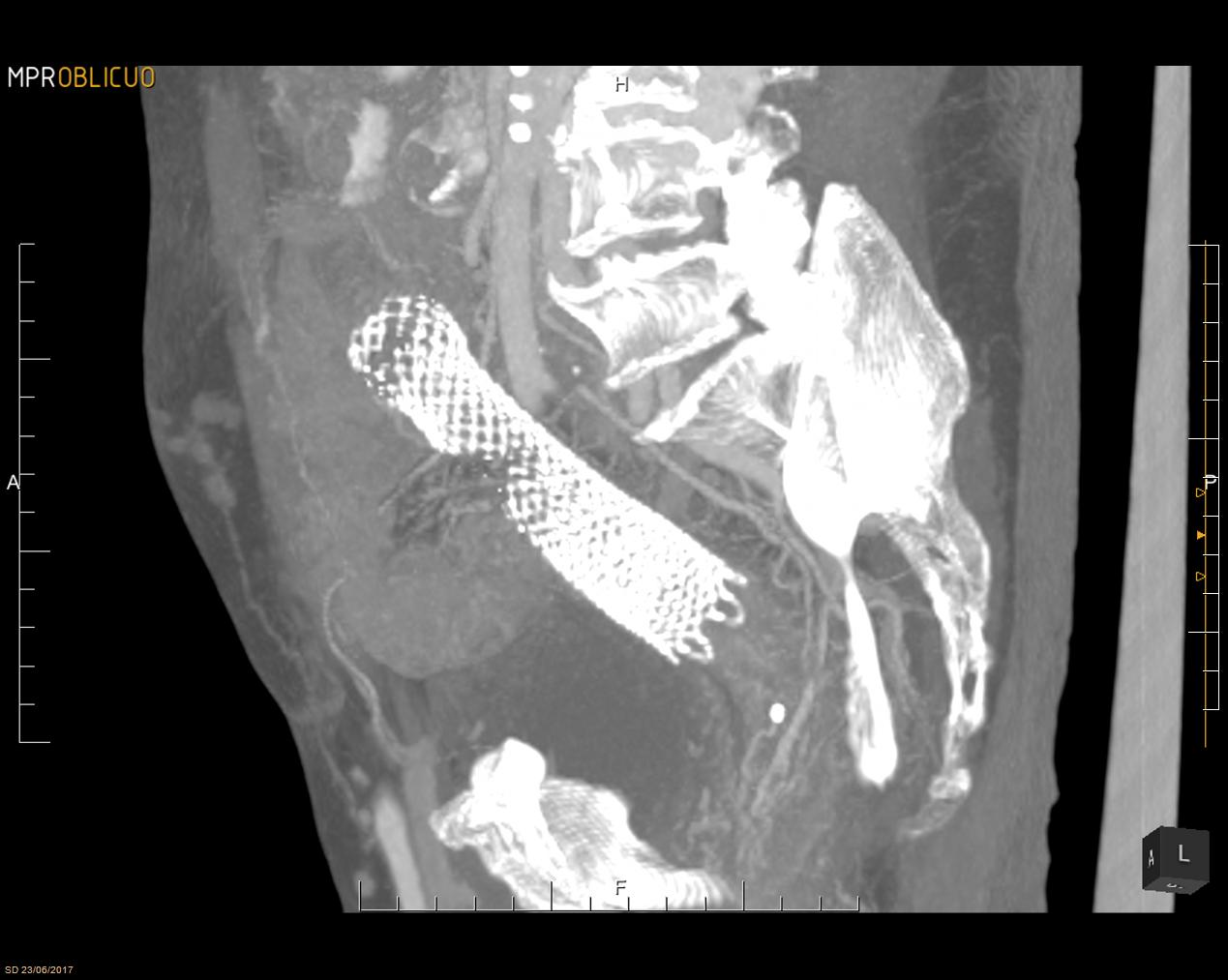 FIG 3.
FIG 3.