To access AIS Channel content, please allow all cookies. Please click here to configure your preferences.
A 73-year-old female patient, with a history of Parkinson's disease. An Endoscopic Gastrostomy Prosthesis was placed with a tube for endoscopic administration of duodopa .
The patient came to the emergency room 5 days later presenting with abdominal pain, distension and feeling poorly overall . A blood analysis was performed, highlighting an elevated CRP with normal leukocytes.
Given the physical examination it was decided to perform an abdominal CT Scan , which showed a dilation of the bowel, more evident in the left flank, at the jejunal level, with a thinning intestinal wall, intestinal pneumatosis and gas in the mesenteric and portals intrahepatic veins . These findings suggested an intestinal ischemia with no identified the cause as the first diagnostic option. A edema in the ileal wall of the bowel on the right flank was a nonspecific finding, but it could indicate an intestinal ischemia at an earlier stage with respect to the previous ones. Gastric distension with liquid content and the presence of a percutaneous gastrostomy catheter entry with a distal end in the jejunum were also found.
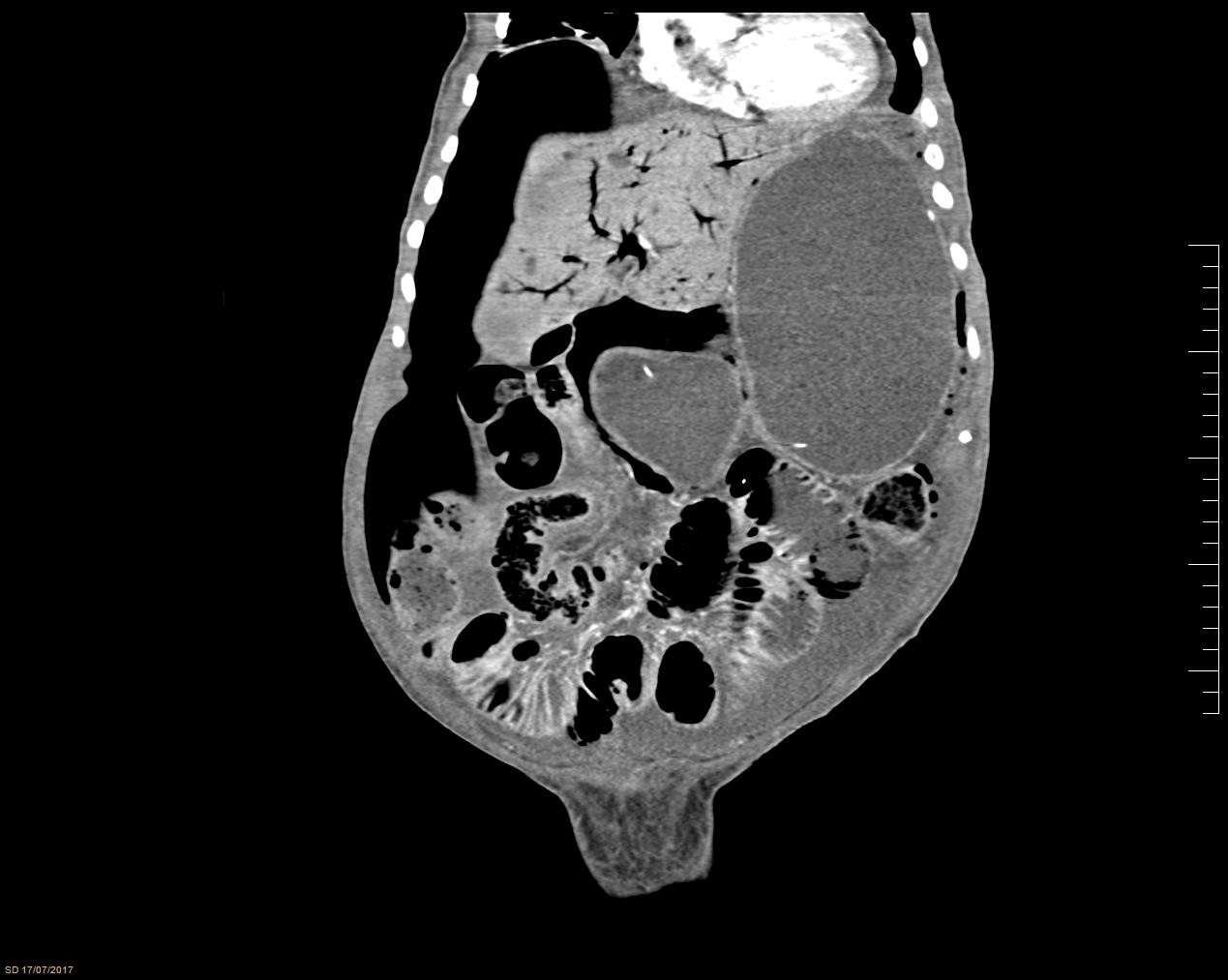 FIG 1.
FIG 1.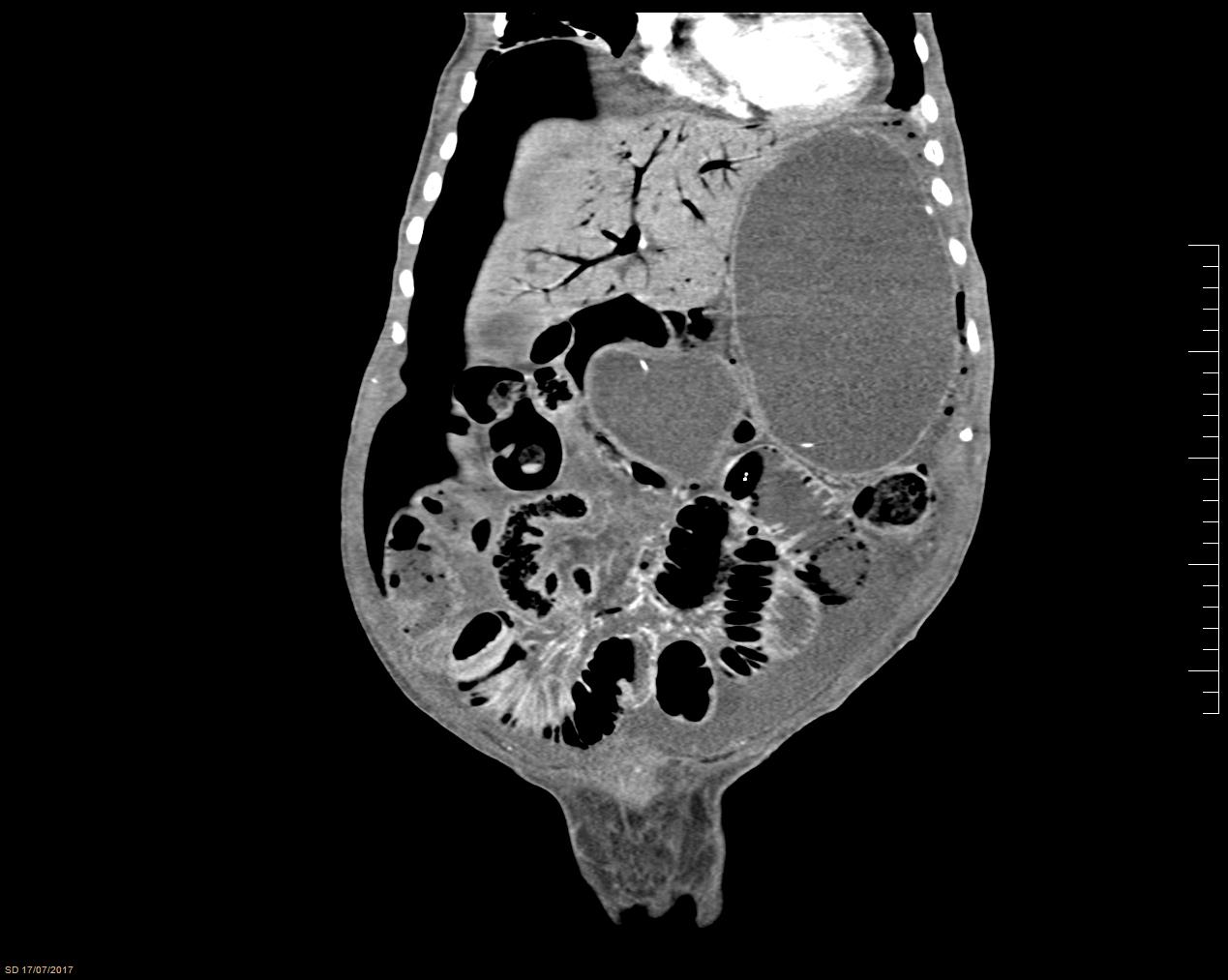 FIG 2.
FIG 2.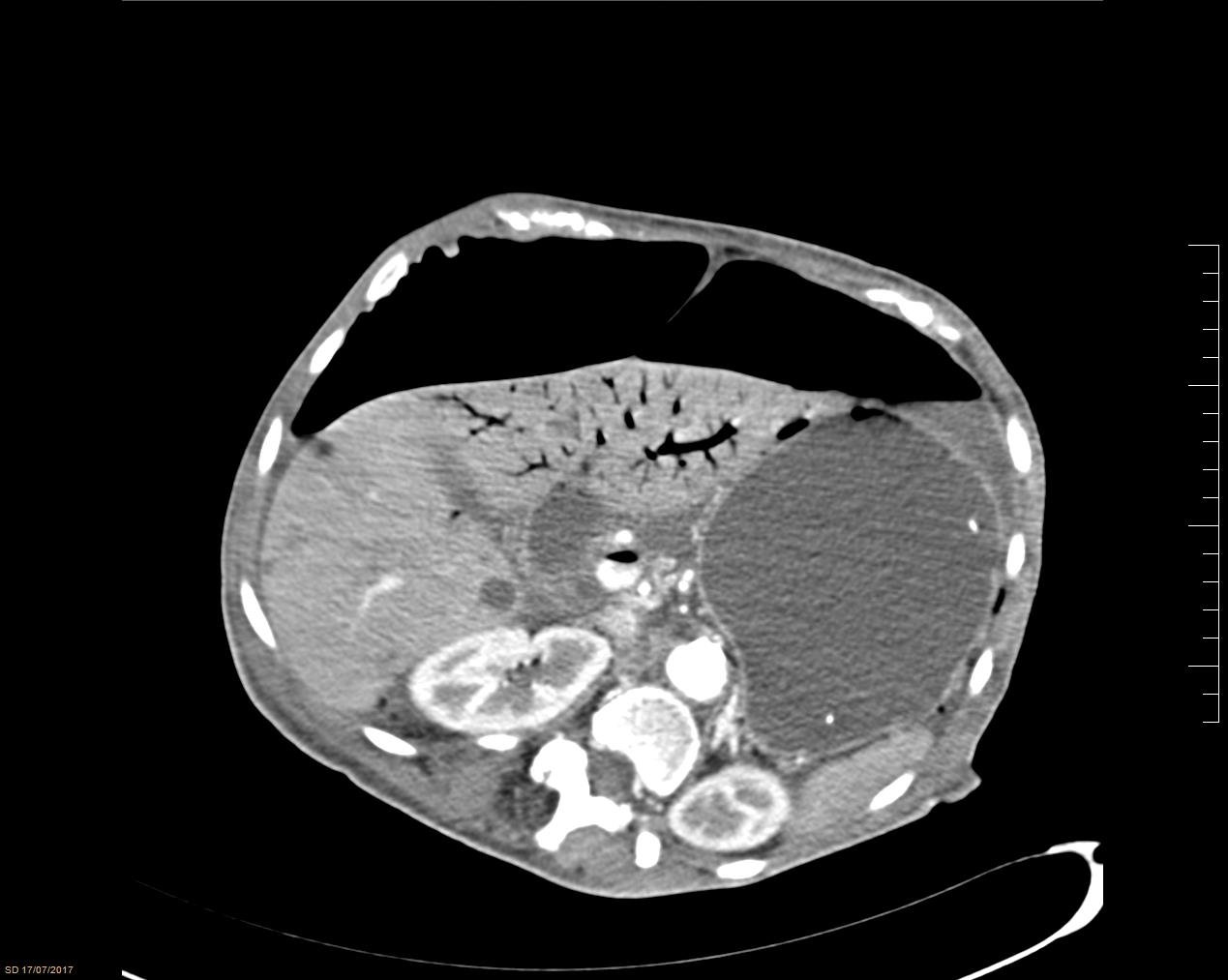 FIG 3.
FIG 3.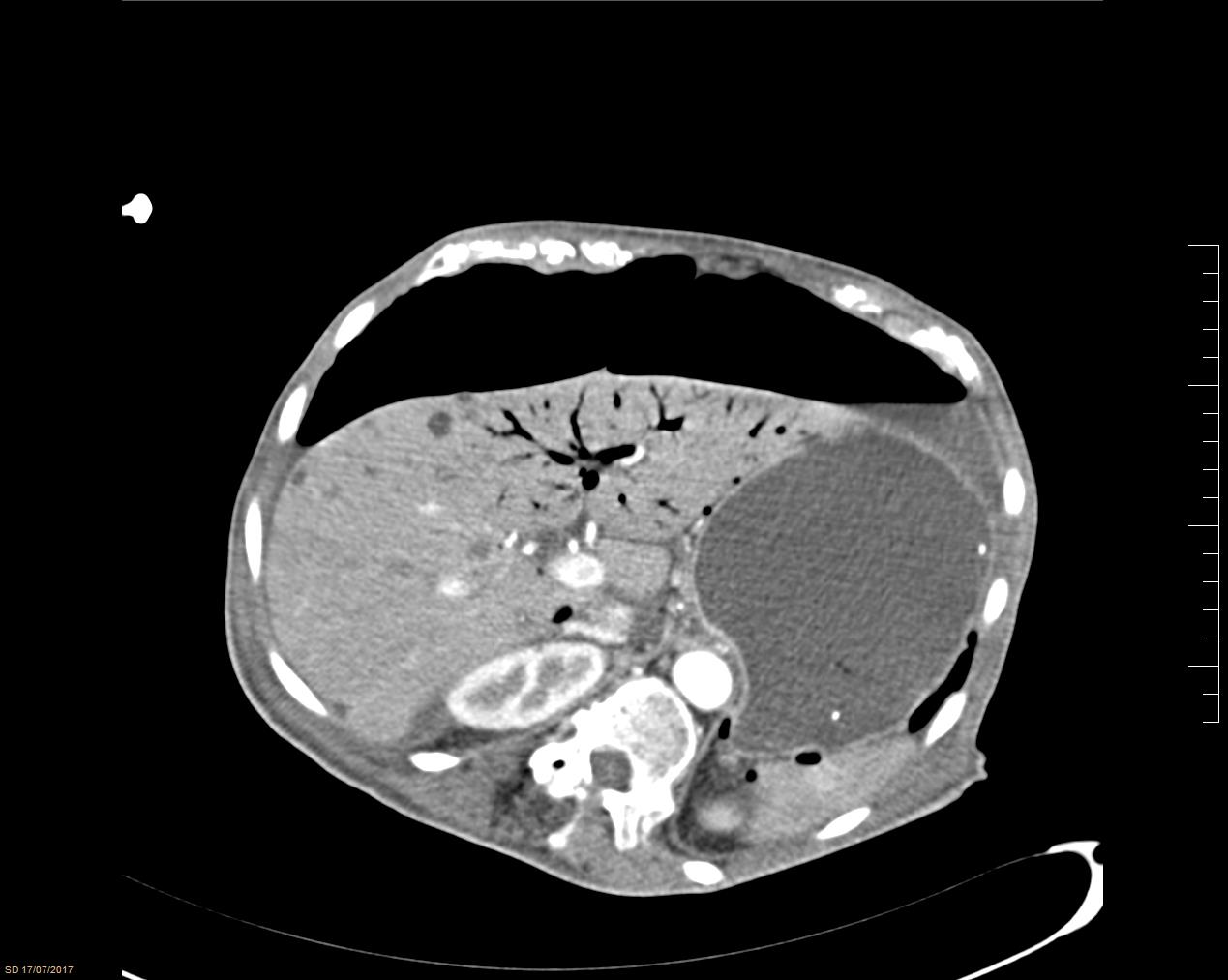 FIG 4.
FIG 4.We decided to perform an emergency surgery.
The patient was hemodynamically unstable, requiring vasoactive drugs. It was decided to perform an exploratory laparotomy.
The findings were consistent with fecaloid peritonitis secondary to leakage of the gastric - intestinal contents around the gastrostomy tube. No signs of ischemia were identified in any organ in the abdominal cavity.
The gastrostomy was repaired with a double suture and fixation of the same to the abdominal wall. In addition, abundant washes of the abdomen were performed and two drains were placed.
The postoperative course was correct, and the vasoactive drugs were gradually removed. The gastrostomy functioned properly and the oral diet was well tolerated.
Portal vein gas is a diagnostic sign which indicates a serious intra-abdominal pathology requiring emergency surgery in the majority of patients. Benign hepatic portal vein gas due to less dangerous diseases can be treated conservatively after the exclusion of an intra-abdominal catastrophe. The correlation between clinical and diagnostic findings is important to design the management plan.