To access AIS Channel content, please allow all cookies. Please click here to configure your preferences.
A 41 year-old-female with a previous history of hiatal hernia and GERD suffered from morbid obesity with a BMI of 40 Kg/m2. She underwent an uneventful LRYGBP, two years later and 20 Kg down she arrived at the emergency room complaining of intermittent abdominal pain and distension that had begun three days before. She had previously visited another emergency department and was discharged with NSAIDs.
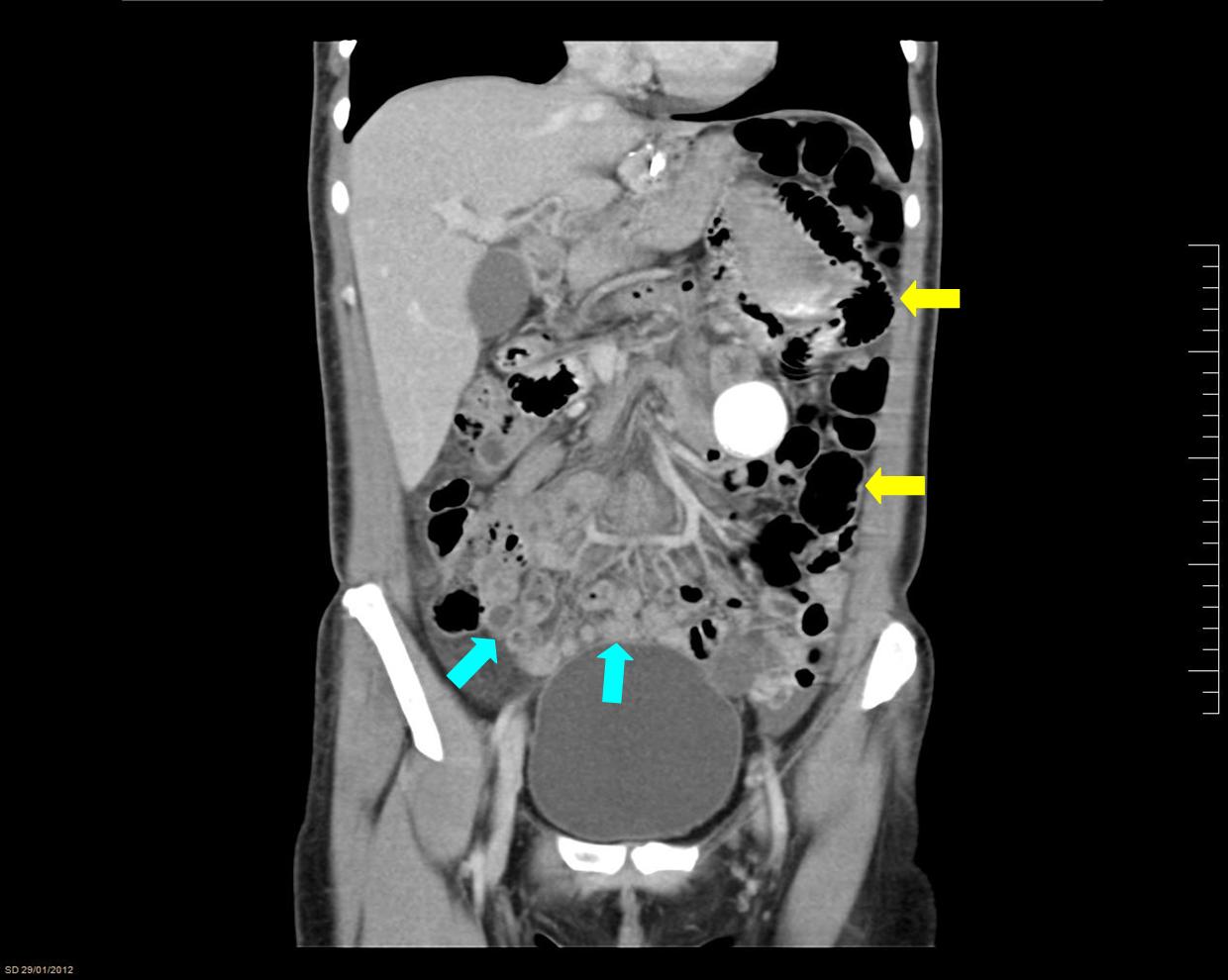
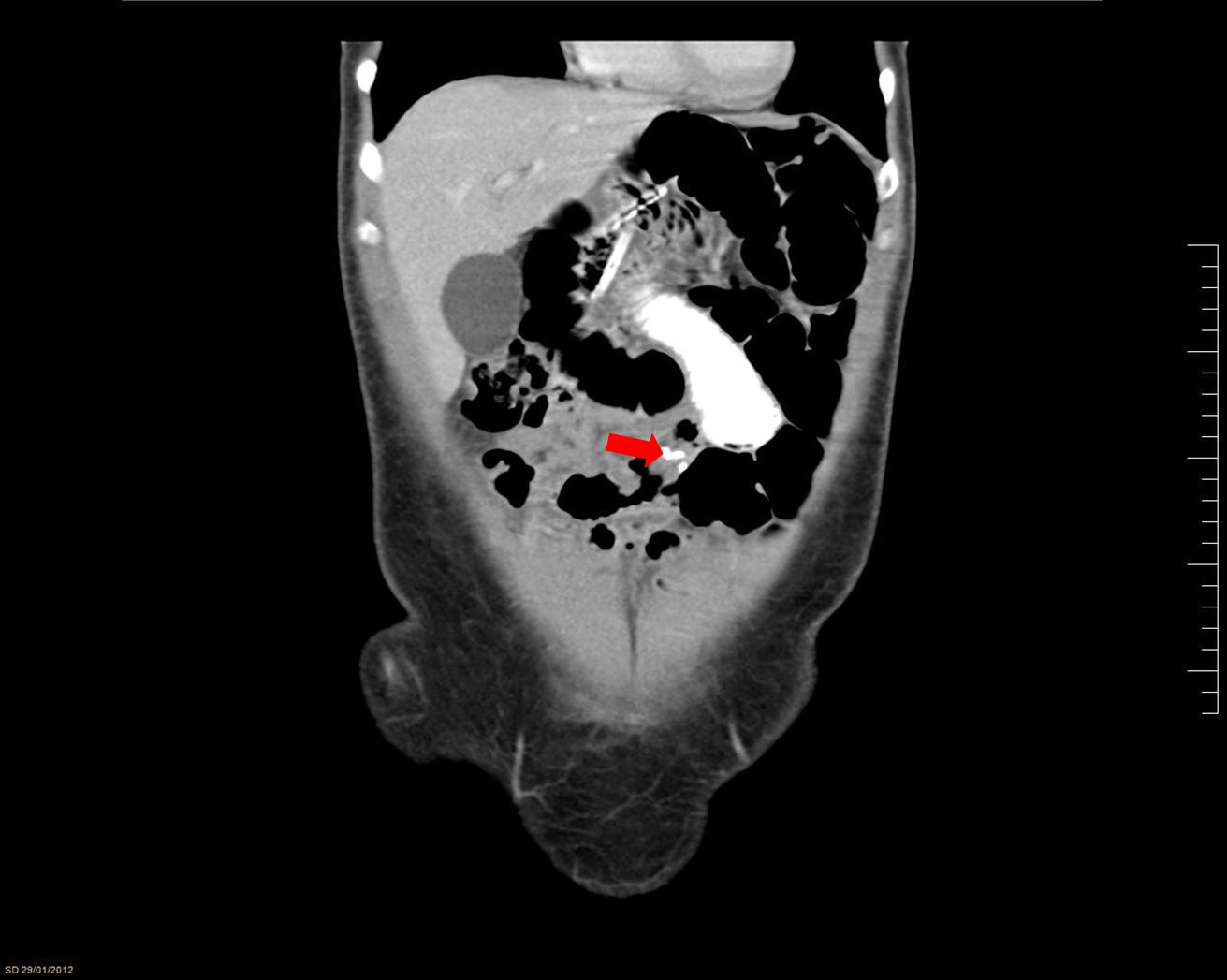
Vital signs were stable, the abdomen was soft with mild pain and bloated on the left flank.The blood test came back normal and the X-ray revealed a distended loop of small bowel. An abdominal CT-Scan with oral and intravenous contrast revealed dilated loops of small bowel at the left flank and some collapsed ones at the inferior right quadrant of the abdomen (FIG. 1). The change in gauge was related to the anastomosis at the level of the foot of the roux limb (FIG. 2). The mesenteric and vessel rotation that is known as the swirl sign due to mesentery and rotation of its vessels was also present (VID. 1). These findings supported the diagnosis of internal herniation.
Laparoscopic revision was carried with the patient in the supine position with open legs, with the leading surgeon and its assistant on the right of the patient. A total of 4 trocars were used: a 12mm trocar in a supraumbilical position for a 30º scope, a 12-mm trocar at the umbilicus, and a 12mm trocar at the right flank. A 5-mm port was placed at the epigastrium.
The alimentary limb was distended and the small bowel was revised from the ileocecal valve to the foot of the roux limb, to avoid performing traction of the fragile and distended small bowel. The internal hernia was reduced exposing the mesentery gap that was closed with a Prolene pursetring. Petersen's defect was closed from the previous surgery. The small bowel was viable and no resection was required.
Surgery took 60 minutes and was uneventful. The patient started oral intake the second postoperative day and left hospital three days after surgery. She remains asymptomatic in the 3rd follow-up postoperative year.