To access AIS Channel content, please allow all cookies. Please click here to configure your preferences.
Introduction
Anticoagulation in patients undergoing surgical procedures is challenging.
Interrupting anticoagulation for a procedure increases the risk of thromboembolism.
Surgery has associated bleeding risks that are increased by the anticoagulants administered for thromboembolism prevention.
First of all, we are going to explain the coagulation cascade in a simple way.
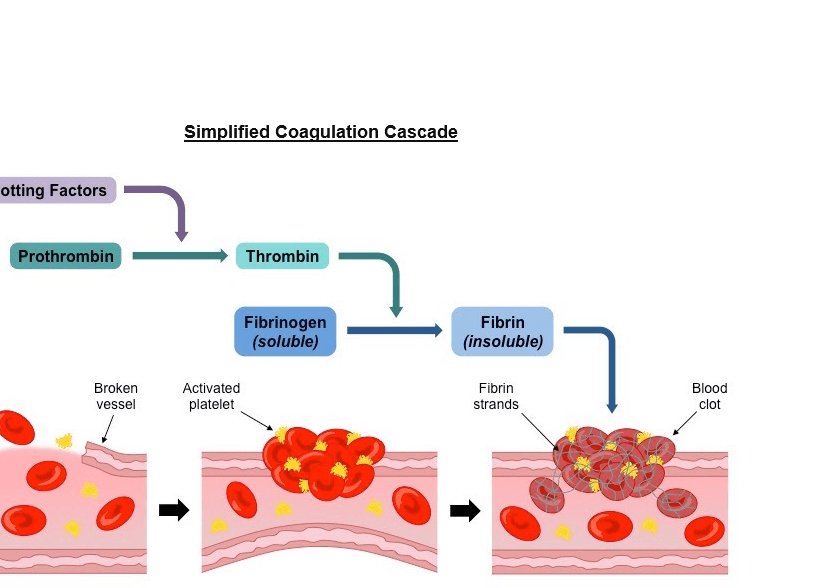
Damaged blood vessel:
Injury to vessel lining triggers the release of clotting factors.
This step changes the prothrombin into thrombin.
Formation of platelet plug:
Vasoconstriction limits blood flow and platelets form a sticky plug.
With the presence of thrombin, the fibrinogen changes into fibrin.
Development of clot:
Fibrin strands adhere to the plug to the form an insoluble clot.
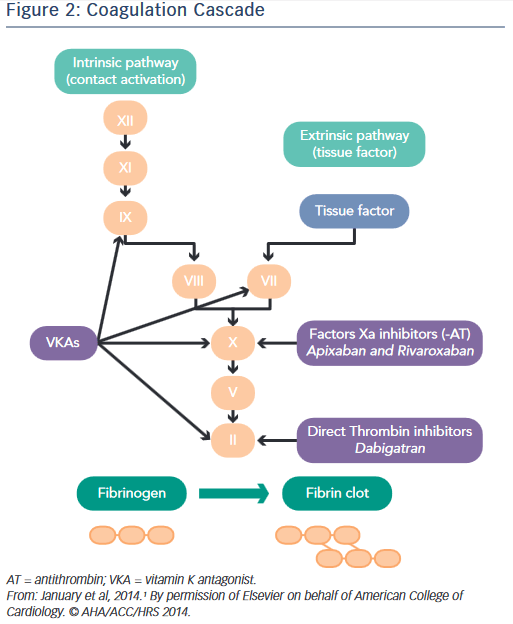
Exists a lot of blood thinners that works in this cascade of coagulation.
Like Warfarin, Direct thrombin inhibitor, Factor Xa inhibitors, etc.
In the case of the Warfarin:
It is used in these pathologies.
This is how the warfarin affects blood clotting.
Warfarin reduces the body’s ability to make vitamin K, which interferes with protein creation.
Lower levels of clotting protein makes blood cells less likely to clot.
The newer direct oral anticoagulants:
This raises concerns about treatment of bleeding and management of patients who require an urgent surgery.
This figure shows the Factors Xa inhibitors: Apixaban and Rivaroxaban and the direct thrombin inhibitors in the factor II : Dabigatran.
Comparison of Warfarin vs Heparin

ESTIMATING THROMBOEMBOLIC AND HEMORRHAGIC RISK?
Annual risk thromboembolic and hemorrhagic.
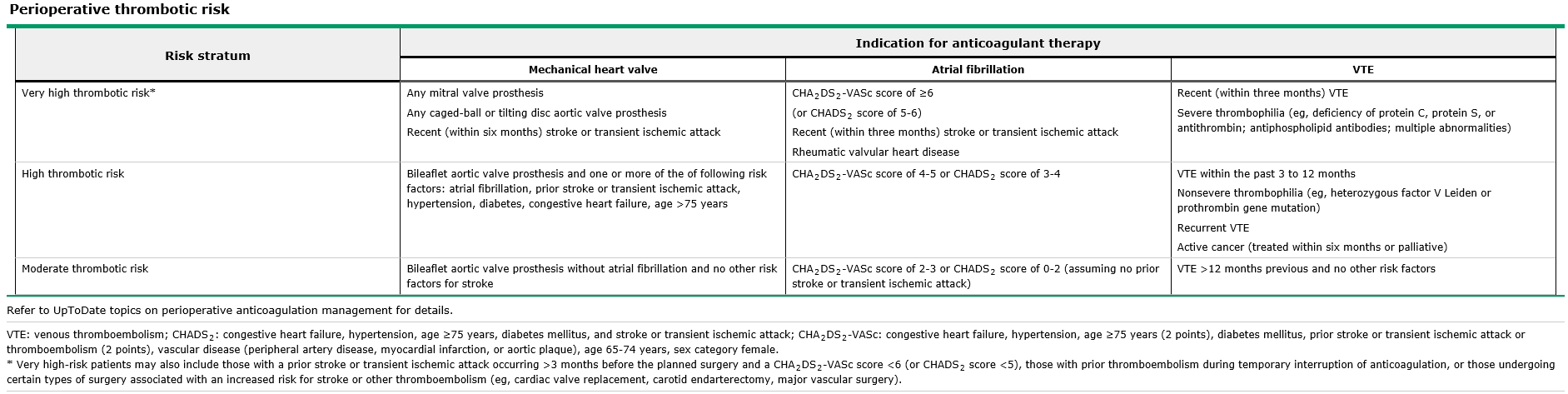
Very high thrombotic risk:
Patients with a risk of more than 10 %, with a mitral valve prosthesis, recent stroke , atrial fibrillation, and recent VTE.
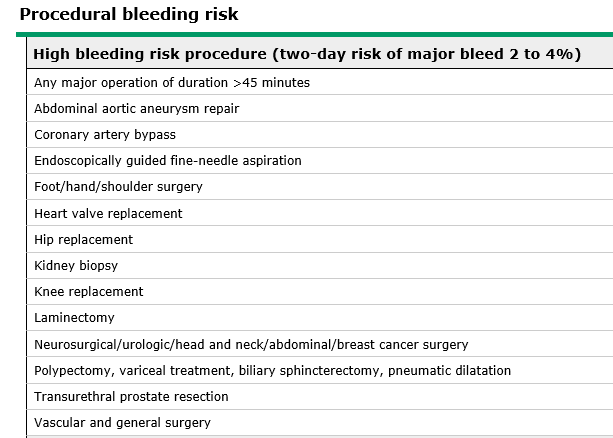
High bleeding risk procedure:
BleedMAP
This is the stratification of perioperative hemorrhagic risk, based on four predictive factors:
BleedMAP => Hemorrhage
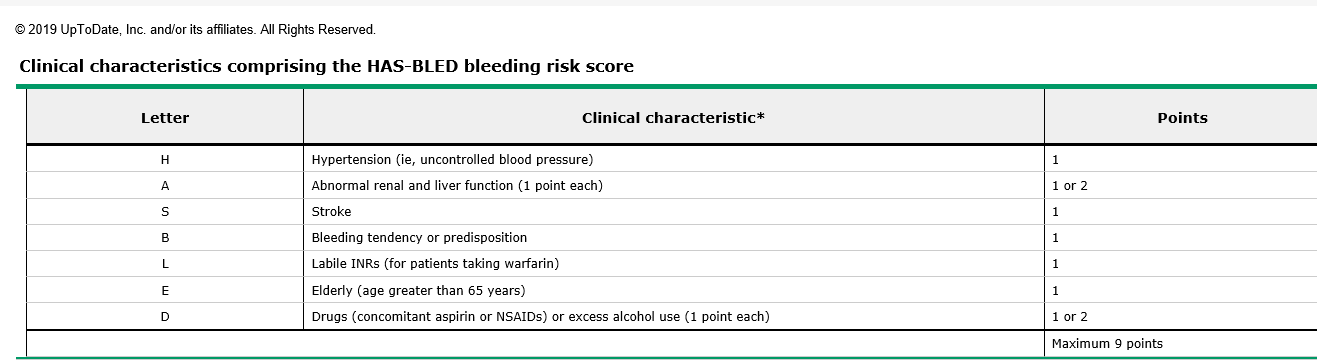
HAS – Bleeding score
Score ≥3 was the most predictive variable for bleeding
DOACs suspension prior to surgery:
If the INR is >1.5, administer a low dose oral vitamin K (1 to 2 mg) to hasten normalization of the PT/INR.
Restarting the drug after surgery:
For patients at very high or high thromboembolic risk, or cases where it is not possible to start oral tolerance, bridging may be appropriate.
Use of bridging PREoperatively:
Therapeutic dosing
Intermediate dosing
Prophylactic dosing
Timing
We discontinue LMW heparin 24 hours before the planned surgery or procedure.
If a twice-daily LMW heparin regimen is given, the evening dose the night before surgery is omitted.
If a once-daily regimen is given, one-half of the total daily dose is given on the morning of the day before surgery.
Use of bridging POSToperatively:
Until there is adequate hemostasis clinical assessment of the wound site, drainage fluid amount, expected postoperative bleeding and correct hemoglobin levels.
This assessment will vary depending on the surgery type and individual patient considerations.
Low bleeding risk
Minor procedures associated with a low bleeding risk in which bridging is used, therapeutic-dose of LMW heparin can usually be resumed 24 hours after the procedure.
Major bleeding risk
Major surgery or those with a high bleeding risk procedure, the therapeutic dose of LMW heparin should be delayed for 48 to 72 hours after hemostasis has been secured.
Resumed
Warfarin is generally resumed on the same postoperative day as the heparin.
Heparin can be discontinued when the INR reaches the therapeutic range (2,0) for individuals at moderate thromboembolism risk.
Perioperative management of the oral direct thrombin inhibitors and factor Xa inhibitors
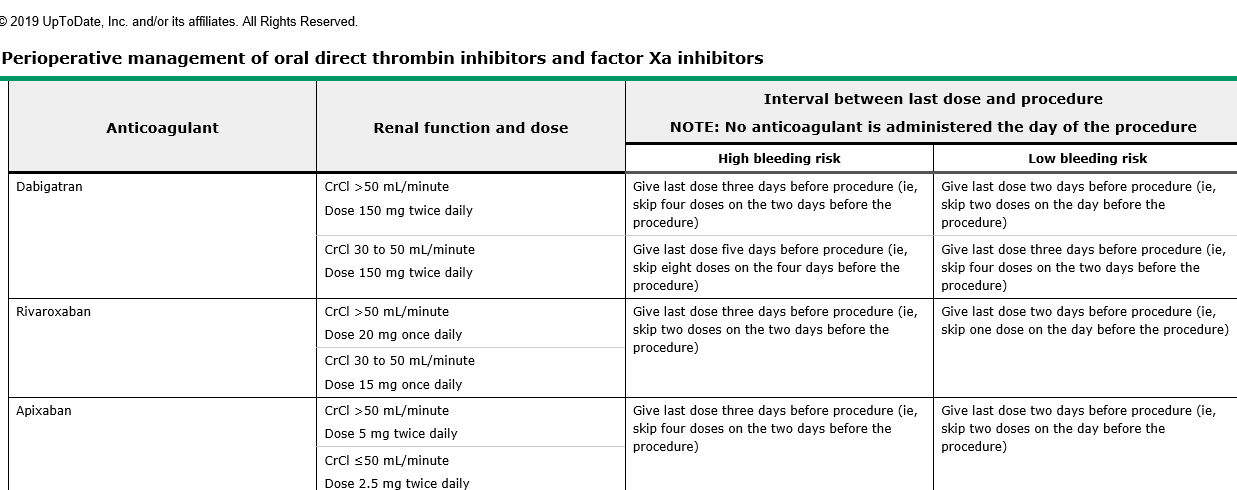
Rapid offset and onset of Dabigatran/Ribaroxaban activity obviates the need for bridging anticoagulation
Dabigatran, Ribaroxaban and Apixaban:
High risk Resumen 48 to 72 hours after surgery.
Low risk Resumen 24 hours after surgery.
Urgent invasive procedure with Warfarin?
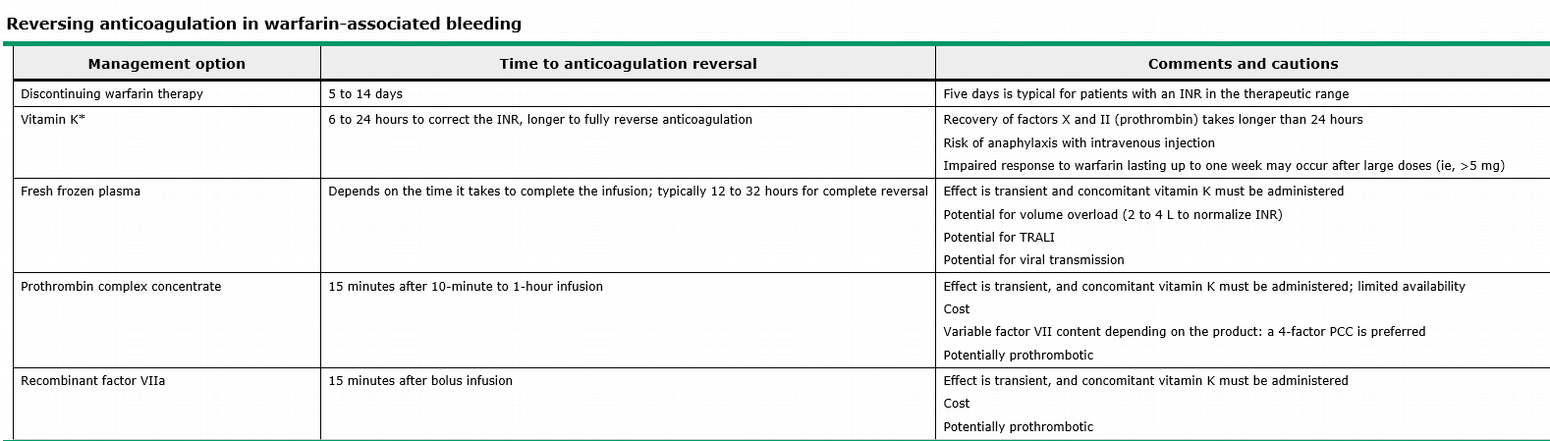
Time to reversal:
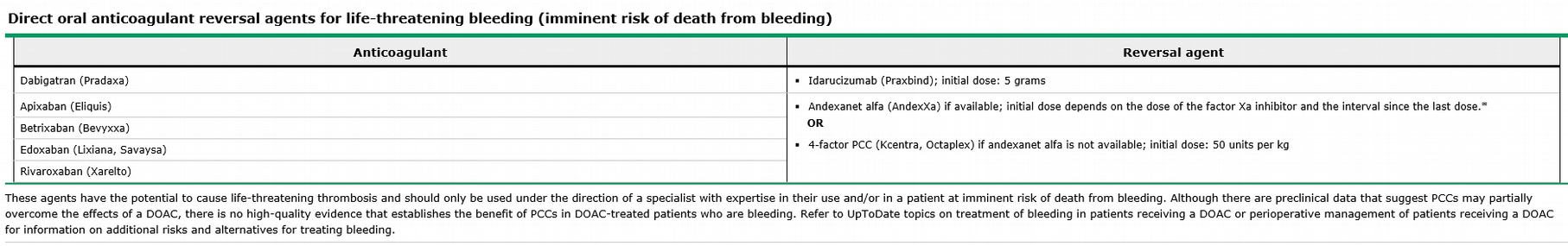
Urgent invasive procedure with Dabigatran/Ribaroxaban?
Take-home messages: